Nursing Homes Are Already Grappling with a Historic Labor Crisis
Nursing homes have been calling for help with staff recruitment and retention challenges for years. Chronic government underfunding has made it difficult to compete for caregivers. The COVID-19 pandemic only exacerbated these staffing challenges, and now long term care faces a historic labor crisis.
Nursing homes are desperately looking to fill vacancies and boost their workforce but there aren’t enough qualified and available candidates. As a result, many nursing homes are limiting the number of residents they can serve or closing entirely.
The Administration’s federal staffing mandate will force more facilities to close or continue limiting admissions if they can’t hire enough caregivers to comply. Currently, 94% of nursing homes do not meet at least one of the four new staffing requirements.
The mandate requires nursing homes to hire more than 102,000 additional nurses, costing nursing homes an estimated $6.5 billion per year — exceeding the $4 billion annual estimate from the Centers for Medicare and Medicaid Services (CMS). This will jeopardize more than 290,000 nursing home residents amid the ongoing labor crisis. Read the full analysis here.
| Nurse Aide | RN 24/7 | RN | Total |
|---|---|---|---|
| 77,202 | 7,274 | 23,931 | 101,757 |
Combination of Requirements Met

Worst Impacted Than Any Other Health Care Sector
Compared to all other health care sectors, nursing homes experienced the worst job losses during the pandemic. While other health care and other industries have largely rebounded, nursing homes have yet to fully recover. Nursing homes still need nearly 190,000 workers to return to pre-pandemic levels—which may not occur until 2026. Read the latest jobs report.

* Assisted Living BLS data through March 2023
Nursing Homes Are Doing Everything They Can, But Need Help
Nursing homes are committed to rebuilding their workforce and supporting their staff. In recent years, they’ve increased wages, benefits and bonuses, as well as boosted assistance, training and career ladder programs. But with fixed government rates, nursing homes lack resources to make additional investments and compete for workers against other employers. As a result, nursing homes are having to ask current staff to work overtime or rely on costly agency staff.
- On average, nurses and nurses’ aides in nursing homes have seen a 17.3% increase in their hourly wages since 2019.
- 95% report difficulties in hiring new staff.
- To cover shifts, virtually all facilities must ask current staff to work overtime and 75% have turned to expensive agency staff.
A Growing Shortage of Nurses
The pandemic and ongoing labor shortage have taken an emotional and physical toll on our nation’s caregivers. Hundreds of thousands have retired or left the profession entirely. At the same time, the nursing gap is deepening—the United States doesn’t have a pipeline of caregivers nor nursing faculty ready to fill the void.
- 100,000 nurses left the workforce during the pandemic. By 2027, almost 900,000, or almost one-fifth of RNs, intend to leave the workforce.
- The U.S. may see a nursing shortage of between 200,000 and 450,000 RNs by 2025.
- In 2022, enrollment in nursing student programs fell for the first time in more than two decades.
How Seniors Are Impacted
The labor crisis is reducing seniors’ access to long term care. When facilities cannot find enough workers, they must restrict the number of residents they can serve. Nursing homes are having to limit admissions, downsize their facilities, and hundreds have closed entirely because of labor shortages.
- 52% of nursing homes are limiting new admissions.
- Nearly one-quarter have closed a unit, wing, or floor.
- 72% are concerned persistent workforce challenges might force them to close.
- There are 600 fewer nursing homes in the U.S. than there were six years ago.
Read the latest nursing home provider survey.
The result: seniors who need care are put on waitlists that are days, weeks or even months long, family members have fewer care options and must travel farther to see their loved one, and hospitals are overwhelmed with patients who should be discharged, increasing costs to the health care system.
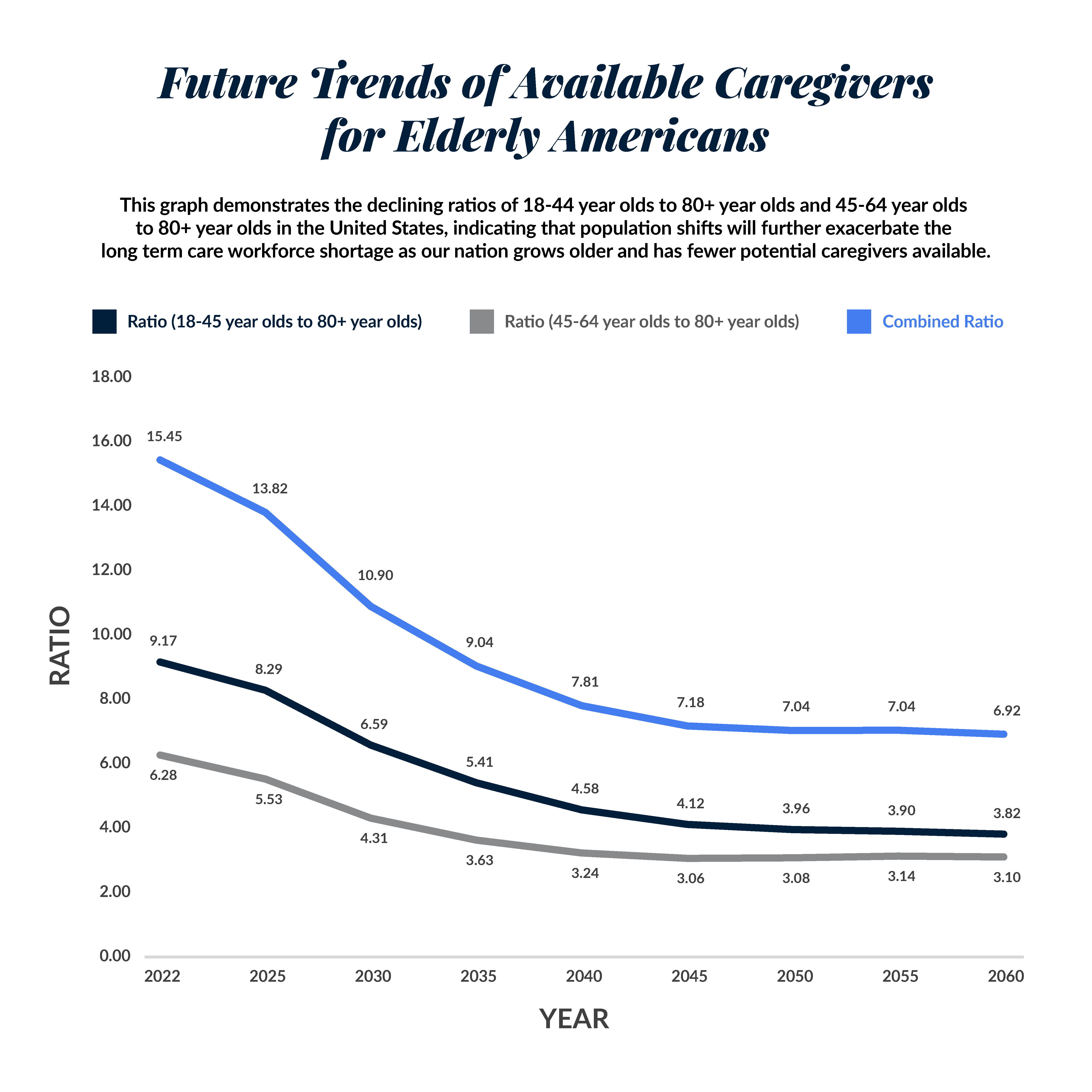
The Silver Tsunami is Almost Here
In the coming years, there will be fewer young people to help care for a rapidly growing elderly population. Comprehensive and innovative solutions will be necessary to respond to changing demographics.
By 2030, all baby boomers will be older than age 65, and one in every five residents will be retirement age. The 80+ population is projected to grow more than 9% between now and 2027. Meanwhile, the number of unpaid caregivers is expected to decrease.
The home care workforce is facing similar labor challenges and is not equipped to absorb an influx of seniors who need around-the-clock care.